My lowest resting heart rate has crept up these past few months. My Oura ring keeps saying that I need to take it easy, but I think I need to do a few more long runs. So I’m going to test that theory.

My lowest resting heart rate has crept up these past few months. My Oura ring keeps saying that I need to take it easy, but I think I need to do a few more long runs. So I’m going to test that theory.
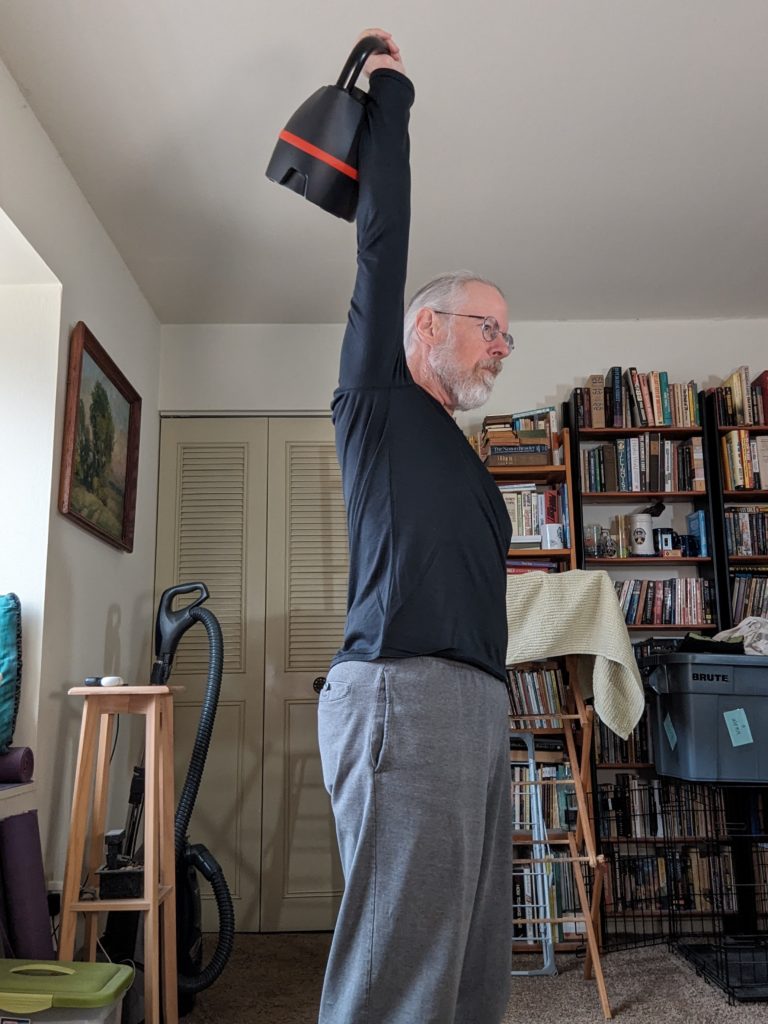
Although I haven’t quite achieved my aspirational goal of doing all the workouts I want to do, I have been getting workouts in, and they’ve been going pretty well. Last week I did my club swinging workout twice, my kettlebell clean & press workout, my kettlebell swing workout, and my HEMA practice all once each.
I’ve gotten this week off to a good start by hitting the fitness room and doing a bodyweight circuit (jump rope, negative pull ups, Hindu squats, Hindu push ups, and my 3-way core circuit) for three rounds, plus some incline press and some dead hangs.
The negative pull ups, in particular, were better than I’d expected. Something I’m doing—probably the kettlebell swings, but perhaps also the club swinging—is working the lats and biceps more than is obvious while I’m doing them.
I’d gotten my workout log notebook out for writing this post, and failed to put it away, with the (dog induced) result visible above.
Based on the ideas that I talked about in Training for everything, here’s my latest cut at a personal exercise program. (My first cut was derailed by circumstances, and then I adopted a dog which derailed everything except dog walking. Then I got West Nile fever.) See my no-longer-particularly-recent Starting to rough up a new training plan for more information about the specific exercises and how I organize them into sets, reps, and progressions.
I have a set of exercises that I want to do, ideally twice a week each:
That’s five things, so if I did each twice, and gave everything its own day, I’d have to have a 10-day week. That isn’t impossible. In fact, I’ve seriously considered planning my workouts in a longer cycle than weekly in the past, it but is unhandy in various ways. Fortunately, I think I can double-up several of these exercises in a way that will let me fit them into 7-day week.
The 1-handed club swinging isn’t particularly intense cardiovascularly, so I’m thinking I can combine it with the clean & press. The KB swings is intense cardiovascularly, but because it’s very different, I’m thinking I can combine it with the gymnastic rings bodyweight circuit, doing the KB swings as a “finisher” after the rings workout.
My HEMA (sword fighting) practice is three times a week, and I can’t adjust that schedule, except by skipping workouts, so I have to work that in when it actually happens.

Of course I also want to get one day a week of complete rest. I’d normally make that Sunday, but there’s a HEMA practice session on Sunday so it’ll have to be on Saturday instead.
So here’s a quick stab at a possible weekly plan:
| Day | Morning | Midday | Evening |
|---|---|---|---|
| Sunday | Rings circuit / KB Swings | HEMA | |
| Monday | 1-H Heavy Club / KB C&P | ||
| Tuesday | Sprints | HEMA | |
| Wednesday | Rings circuit / KB Swings | ||
| Thursday | 1-H Heavy Club / KB C&P | HEMA | |
| Friday | Long run | ||
| Saturday | Rest |
I’ve omitted a “warm-up” block, because I already do my morning exercises, my ridiculously long warm-up routine, nearly every day. I’ve also omitted my dog walking, which averages something over 6 miles a day.
I’m pretty happy with this. It has my HEMA practice sessions in at the correct times; it leaves open the time slots where I have Esperanto, and meeting friends for lunch; it has a full rest day.
I don’t show it here, but I’ll definitely do a de-load week every 5 or 6 weeks.
I should be very clear that, at this point, this is entirely aspirational. I’ve been doing each of these workouts individually, but the only combined workouts I’ve tried so far are the heavy club swinging and the clean&press workouts. I’ve also been taking more than one rest day per week. But the progress I want seems to depend on doing something like this workout schedule, so I’m going to give it a try.
I’ll report back regarding my success or failure.
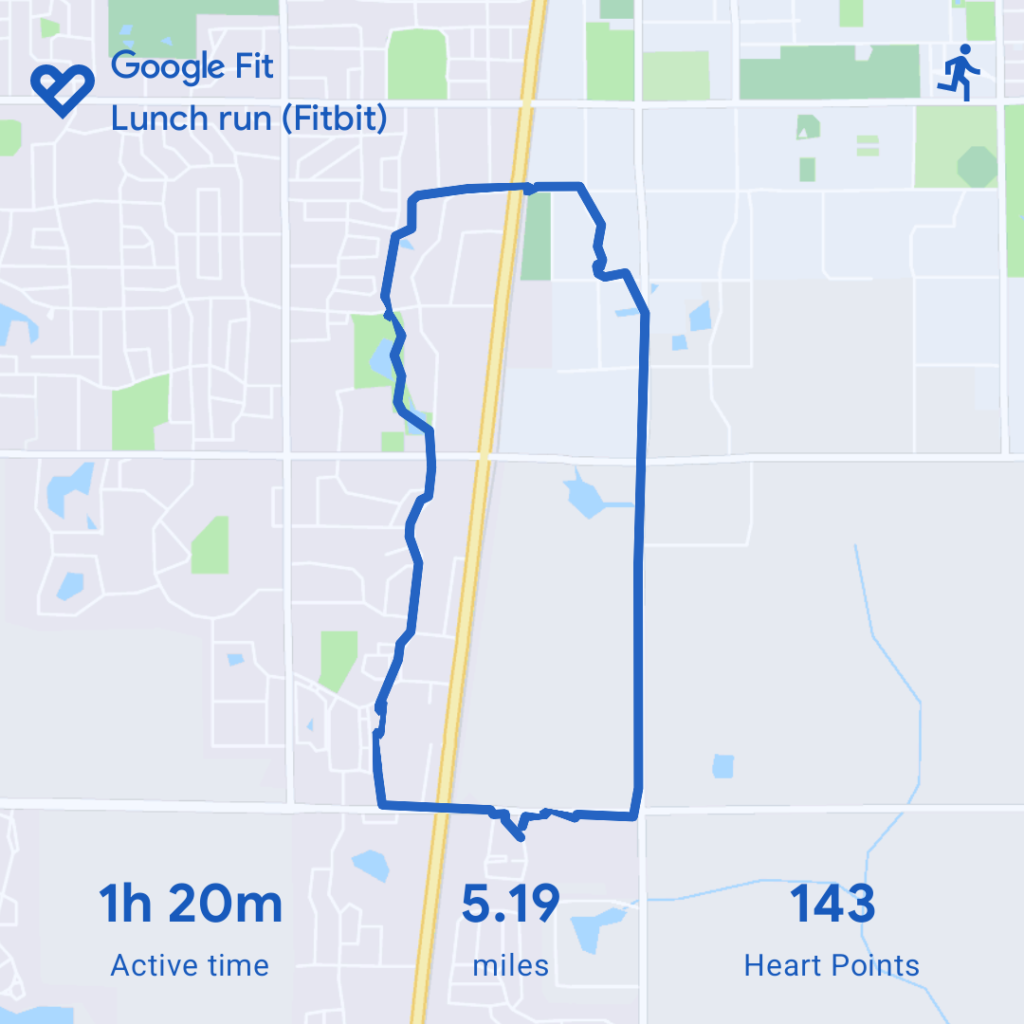
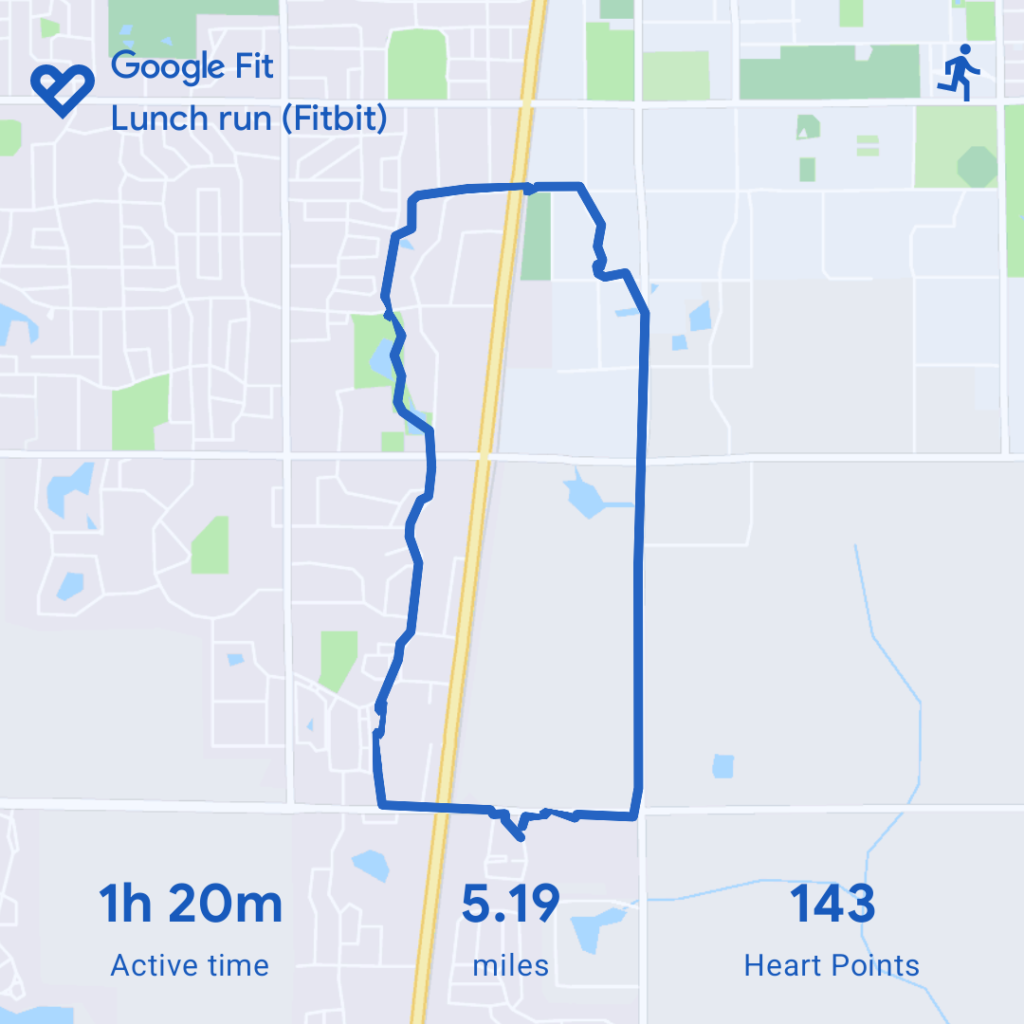
That’s more like it! My first few runs after having been sick were pretty mediocre, but today I ran 5.19 miles in 1:18:28, and felt good right on through. 🏃🏻♂️

I’ve felt entirely recovered from West Nile fever for going on three weeks now, and I’ve been going back to my HEMA training sessions. But until today I’ve been finding that, once I finished the actual class part of the class, I was all worn out, and didn’t feel up to sparing. But today, I felt like I could spar. So I did.
I didn’t get any video unfortunately, but I did spar with two different people, and managed to get some hits. It was good. I’m not going to beat anyone who’s any good at fencing, but that’s okay at this point. The main thing is that I’m finally, once again, able to train for an hour and a half and then spend half an hour sparing.
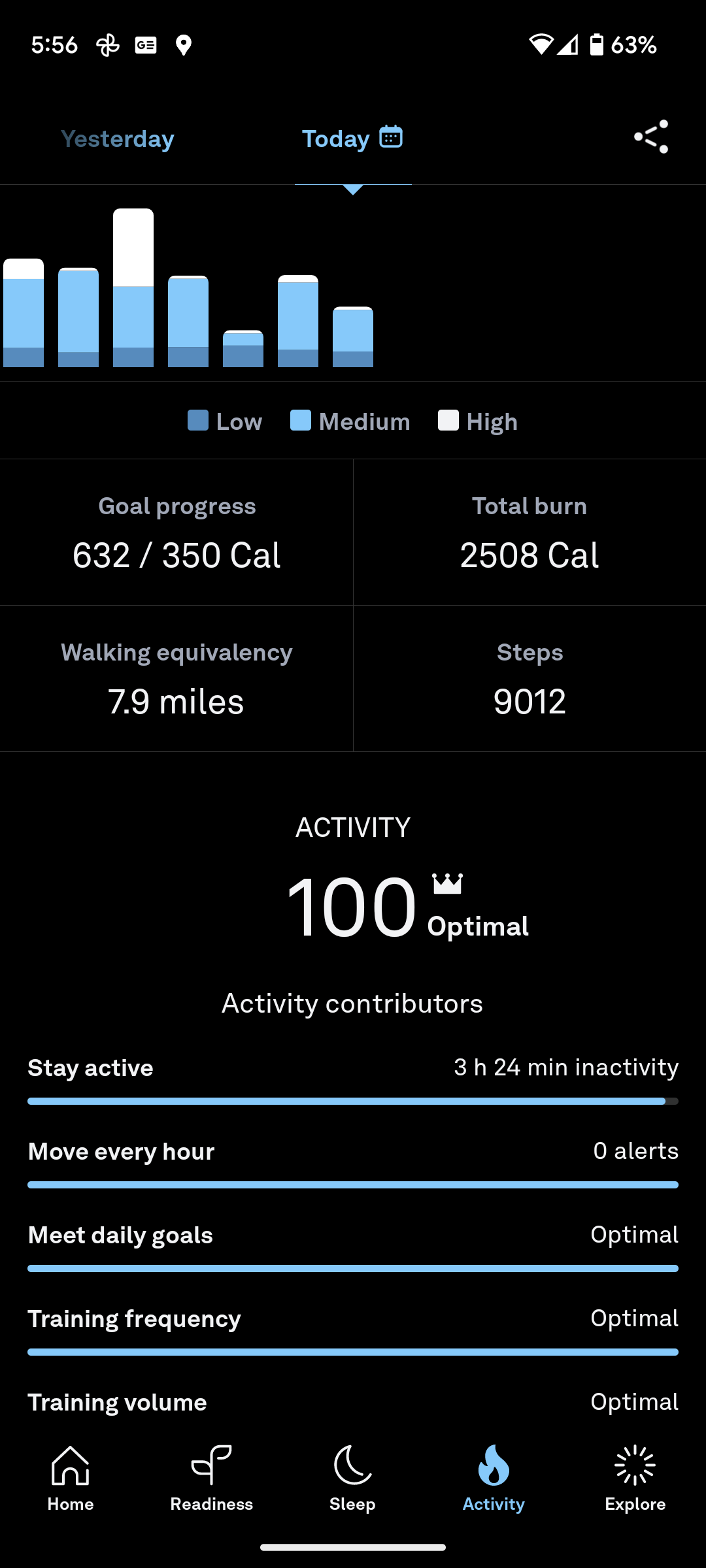
Oh, and two related details. One from my Oura ring which give me a score of 100 for my activity today:
And from fitbit on my Pixel watch, yesterday I got the Sahara badge, meaning that since I bought my Pixel watch (October 2022) I’ve walked the length of the Sahara desert (2983 miles):

I’ve had a draft post that was originally called my “fall workout plan,” and then called my “late fall workout plan,” but that I never posted because while I was sick I couldn’t work out at all, beyond walking the dog. I will post it. Perhaps not until it makes more sense to post a “winter workout plan.”
In the meantime though, I am, finally, back to doing workouts, and thought I might talk about what I’m doing, because my workout plan is to do workouts very similar to what I’ve been doing over the past week or so.
Back at the end of September I came down with West Nile Fever, which made me pretty sick for a long time. The only time in my life before I was that sick for that long was when I had Mononucleosis when I was a freshman in college. That time I was sick for most of the term, and it took several weeks of the Christmas vacation to fully recover.
With West Nile it took about three weeks to recover from the acute phase of the illness. That is, I had a fever constantly for three weeks. Then it took another three weeks to get my energy levels back. For that period I could walk the dog, fix breakfast, and then do one thing, after which I needed to go back to bed and take a nap.

As of a couple of days ago, I think I’m back to full health. I’ve been doing workouts—not as frequently as I’d like, but often enough that I’ve been able to start pushing the weights up again, although not up to what I doing before I was sick. I’ve been for a couple of runs, both of which were harder and slower than I’d like, but were okay—I didn’t feel like I was sick, just like I hadn’t been running enough the past few weeks.
On Sunday I got a Covid booster, so I felt slightly less energetic Monday, but that has already passed.
After too many weeks, I finally feel back to normal!
Because I use wearables to capture as much information about myself as possible, I can go back and see how my illness affected my activity.

Between returning home from vacation in August, and getting sick in late September, I averaged between 6 and 8 miles a day, mostly walking the dog. (Separately I got in a run each week, pushing that day’s mileage up over 10.) In October (as you can see above) my distance fell to between 3 and 4 miles each day until just about the middle of the month, then gradually started increasing. I exceeded 6 miles on October 15th. I didn’t reach 8 miles until October 30th.
Now I’m right back to 6 to 8 miles a day, same as before I was sick. And today I went for my first run since September 26th. It was a pretty crappy run, but better than not running.
Today I managed to get in a workout—my first since coming down with West Nile fever five and a half weeks ago. (I dropped the weight by 33%, and dropped the set count by almost 50%, but I did do the whole workout I’d planned.)
I was only really sick for about 3 weeks, but oof—it has sure taken a long time to go from “mostly better” to “well enough to exercise.” The past two and a half weeks just fixing breakfast and walking the dog left me so tired I had to take a nap.
Hopefully I’ll be able to get back to regular exercise now, and go back to sword fighting!